Successful treatment of infectious diseases requires an accurate diagnosis of the causative pathogen and an understanding of how susceptible the pathogen is to the antimicrobial agent/s that can be used to treat the infection. In recent decades however, infectious pathogens (fungi, bacteria, viruses, and parasites) have slowly developed resistance to first-line antimicrobials, consequently making them difficult to treat and requiring the use of more potent second-line antimicrobials.
Typically, these more potent drugs are kept in reserve and only used as a last resort. If pathogens become resistant to these potent drugs, we may be unable to treat some infections and reverse the successes achieved in the fight against infectious diseases.
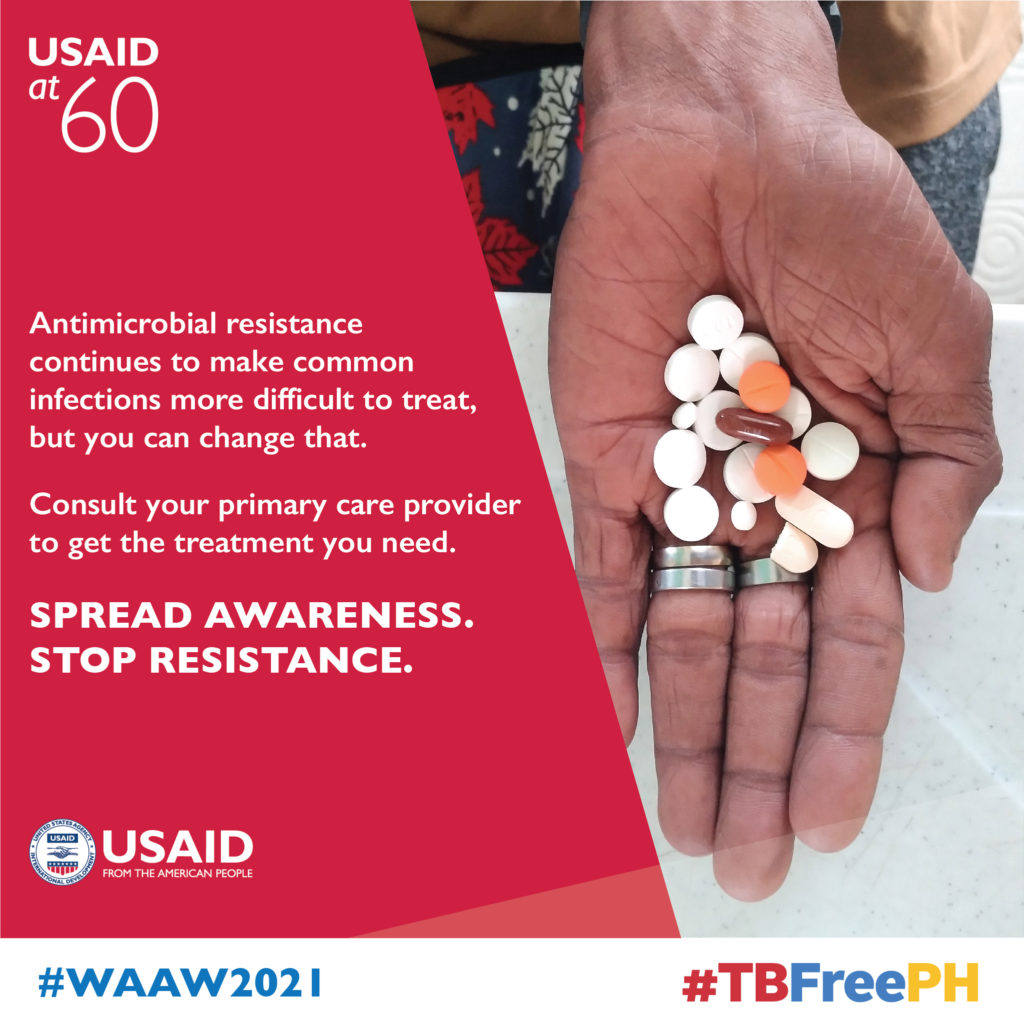
Antimicrobial resistance (AMR) occurs naturally as infectious pathogens can adapt to their environment. However, it is exacerbated by inappropriate (misuse) and excessive (overuse) use of antimicrobials in the human healthcare, animal, and agriculture sectors.
Misuse of antimicrobial agents occurs when humans or animals take drugs when they are not supposed to. For example, in many resource-limited settings, people can and usually prefer buying drugs (such as antibiotics) from chemists or pharmacies without getting a prescription or seeing a doctor first. In such situations, if the infection is viral, no benefit will be achieved from taking antibiotics.
On the contrary, the normal healthy bacteria in the patient will be exposed to antibiotics and may develop resistance. In other instances, patients pressure doctors to prescribe antibiotics when perhaps they are not needed. Counterfeit drugs are also a problem as often they don’t contain the right amount of active antibiotic which can lead to AMR. In addition, stopping antibiotics before the course is complete can lead to AMR.
Antimicrobial’s overuse is also seen in animals reared as a food source. Due to the rapidly increasing demand for livestock products driven by human population growth, the traditional way of producing these animals is being replaced with modern animal rearing habits such as exposing food animals to antibiotics to enhance growth. This involves adding antibiotics in animal feed to increase efficiency and growth promotion.
In chicken feed, for instance, select antibiotics have shown substantial improvement in egg production, feed efficiency and hatchability, and a lower rate of disease spread and/or deaths in the event of an outbreak. For instance, in a recent study in Denmark, 40% of fresh pork sampled was found to contain antibiotic resistant bacteria. Therefore, when humans consume products from animals that have consumed antibiotic-containing feed, this exposes the person to the antibiotics which can also lead to AMR.
According to the World Health Organization, AMR currently accounts for more than 700,000 deaths per year internationally. If no meaningful measures are taken to contain its progress, AMR will cost approximately 10 million lives and about a trillion US dollars per year by 2050. However, in Africa, the actual AMR burden is hampered by inadequate drug resistance surveillance data which is limited to only a few countries. According to a recent article, AMR data is not available for 42.6% of countries in Africa. Nonetheless, available data suggests that Africa shares the worldwide AMR burden.
A highlight of key factors compounding the AMR burden in Africa
- Weak governance systems: lack of policies and guidelines such as those for antimicrobial stewardship. In some cases, the guidelines are available but not implemented due to constrained resources. This is sometimes associated with access and use of pharmaceuticals of doubtful quality.
- Weak diagnostic networks and stewardship: very few laboratories have the capacity to offer appropriate and often complex AMR testing methods which leads to clinicians opting not to collect specimens for AMR testing.
- Weak surveillance systems: very few laboratories are tracking commonly identified organisms in each hospital or location as well as evolving antimicrobials sensitivity or resistance patterns to inform prescription practices.
- Other factors include a lack of continuing education on antimicrobial use (AMU) for prescribers, the tendency for animal owners to stock drugs and engaging unskilled people to treat animals, and a high degree of drugs abuse by livestock keepers and unregulated disposal of waste in dumps.
Other factors include a lack of continuing education on antimicrobial use (AMU) for prescribers, the tendency for animal owners to stock drugs and engaging unskilled people to treat animals, and a high degree of drugs abuse by livestock keepers and unregulated disposal of waste in dumps.
FHI 360’s contributions to mitigate the AMR scourge
FHI 360 acknowledges that addressing the AMR problem requires interventions using a One Health approach. We collaborate with donors, country governments, and in-country stakeholders to implement targeted remedies within the human, animal, and environmental health sectors.
For example, through the U.S. Agency for International Development (USAID) funded Infectious Disease Detection and Surveillance (IDDS) project, we have supported fourteen African countries to strengthen their diagnostic and surveillance systems for AMR including Tuberculosis (TB) and zoonotic diseases. Furthermore, our support has led to development and implementation of an AMR Surveillance curriculum that aligns to the One Health approach, which is helping to address the AMR/AMU knowledge gaps. We have also strengthened both human and animal health laboratories to implement quality management systems including supply chain systems for AMR surveillance which has resulted improved clinicians’ confidence on AMR tests leading to demand creation.
Additionally, our work in Kenya has led to international accreditation of two human health laboratories while we continue to provide technical support to four animal health laboratories in Uganda to achieve accreditation. Our AMR response and containment support work for the last two years has led to at least three (Ethiopia, Kenya, and Tanzania) countries sharing AMR data to the World Health Organization’s Global Antimicrobial Resistance Surveillance System (GLASS) for the first time.
Through the USAID funded Medicines, Technologies, and Pharmaceutical Services (MTaPS) project, and via implementation science projects, we have contributed to the development or review and updating of Antimicrobial Stewardship (AMS) and Infection Prevention and Control (IPC) guidelines in thirteen African countries. Our contribution has led to review and updating of essential medicines list and development or review and updating of antimicrobial use (AMU) guidelines for the supported countries.
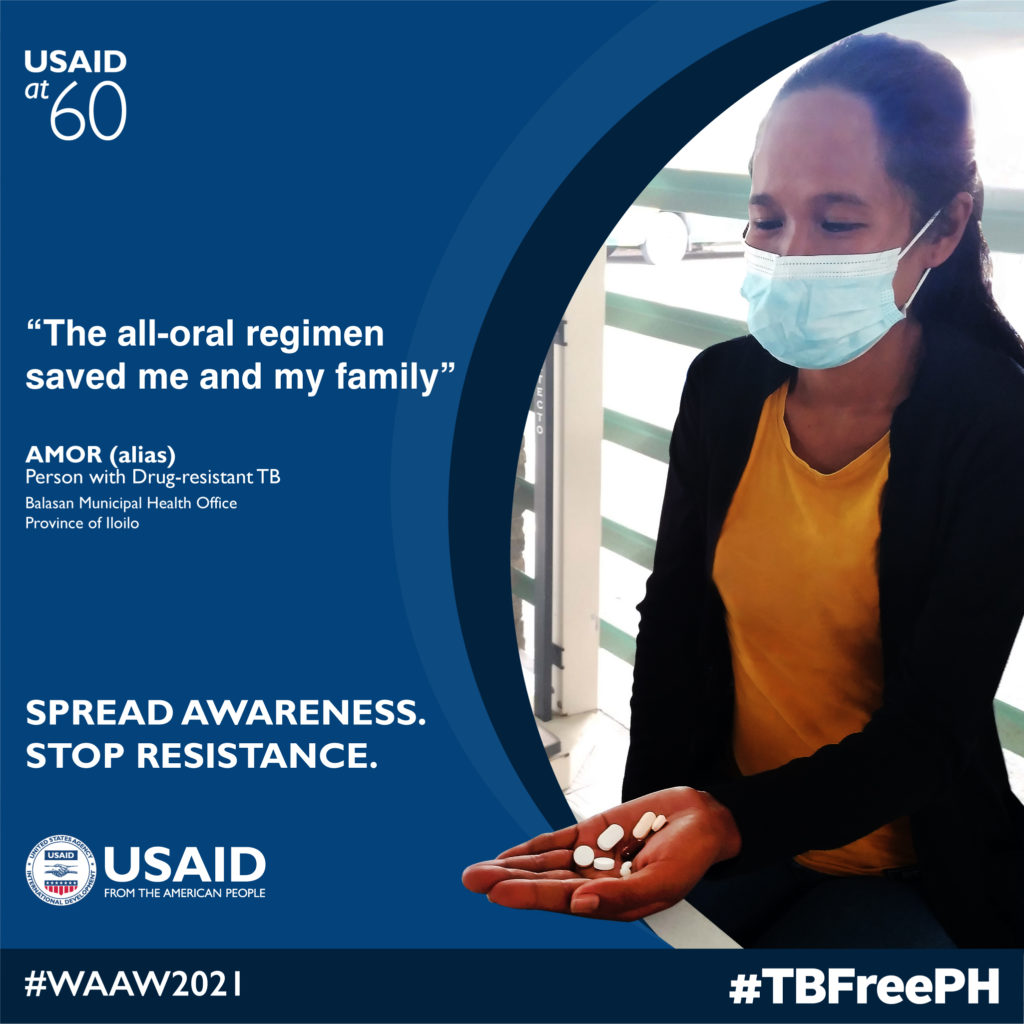
From our partners at USAID: World Antimicrobial Awareness Week 2021